1 Harvard T.H. Chan School of Public Health, Boston, MA, USA; 2 Harvard Medical School, Boston, MA, USA; 3 Department of Medicine, Division of General Pediatrics, Boston Children’s Hospital, Boston, MA, USA
Journal MTM 6:2:47–55, 2017
Background: Despite the growth in smartphone use among adolescents, few mobile health applications (apps) – apps designed to support general health management – are designed specifically with this population in mind.
Aims: To explore adolescents’ perceptions regarding the use of smartphone apps for health management using qualitative methods.
Methods: Inductive thematic analysis of 20 individual semi-structured interviews exploring 1) experience with health-related smartphone apps, 2) perceived barriers to, and 3) facilitators to app use.
Results: Of the 20 participants, 55% were male, 40% Latino, and 50% Black, with mean age of 15.1 years (SD=1.7). Forty percent had used health apps for tasks such as managing a medical condition or achieving a fitness goal. The overall “look and feel” of apps impacted adoption. Barriers to use included low awareness, competing priorities, and negative impressions, including the perception that health apps were designed primarily for adults. Facilitators to use included general features of the app (interface design, multimedia content, customizability, and rewards) and social influence.
Conclusion: The experiences, attitudes, and preferences regarding health apps uncovered from this study may inform future mobile health interventions targeting adolescents.
Mobile technology usage has grown exponentially since the introduction of smartphones, fueling an explosive proliferation of companion applications (apps). 1 Smartphone penetration is high among younger demographic groups, with 73% of adolescents aged 13–17 years in the United States having access to a smartphone and 58% having downloaded apps. 2 , 3 Mobile health interventions using smartphones are increasingly deployed in clinical settings to augment patient education, communication, monitoring, and chronic disease management, 4 and there are currently thousands of commercial smartphone “health apps”— apps designed to support health management.
The advantage of smartphone apps over traditional approaches to health management, particularly among the younger, tech-savvy generation, is that they provide an interactive, social, and personalized platform to help users modify their own behaviors with minimal professional contact. 5 Since devices accompany users at almost all times of day, users can seamlessly integrate health monitoring into their daily schedules. Because apps can be widely disseminated across socio-demographic groups, 2 they may address barriers that have historically impeded health change among teens, such as time constraints, convenience, social factors, motivation, and access to care, 6 , 7 thus filling gaps in addressing disadvantage or diversity. Apps can also tackle various aspects of health, including diet, exercise and various modes of behavior change through motivation via role models (stages of change) and addiction theories. 28 An individual can therefore find an app that applies to their specific health needs.
Despite a growing body of research on health-related smartphone applications, there is a gap in understanding how this technology pertains to adolescents. The majority of studies to date has targeted adult populations, 8 and as a result, may not be relevant to adolescents, who could have distinct technology usage patterns. 2 In addition, research has focused primarily on efficacy under ideal “laboratory” situations rather than effectiveness in real-world settings, 8 – 11 and may overestimate users’ “natural tendency” to adopt smartphone apps. Even under optimal conditions, studies have demonstrated low user engagement and poor adherence. 8 , 11 A fundamental flaw underlying poor uptake in health app interventions may rest at the core of the design process; a systematic review discovered that only 22.5% of studies involved target users or relevant stakeholders prior to the development of apps. 10 Further studies that have attempted to understand adolescent usage patterns of mobile apps for health have found that on a broader scale, it is important to understand how social media can affect adoption of health apps, emphasizing the need for clearer understanding of the factors that influence long term uptake. 28
Eliciting adolescents’ motivations for using an app is important because that determines how to tailor an app to the user to promote continued usage. 29 Since few studies have focused on teenagers’ pre-existing attitudes towards health apps, we collected qualitative data to better inform app developers and healthcare professionals about adolescents’ perspectives and biases towards using smartphone apps for health management in general. Specifically, we wanted to learn about 1) teens’ experiences with health apps, 2) barriers to, and 3) facilitators to health app use. Gained insight may inform future strategies involving this promising technology.
This study was performed during well-care visits at the Boston Children’s Hospital Primary Care Center at Longwood (PCC-Longwood) from February to April 2015. The PCC-Longwood is an urban academic practice that annually serves 15,000 children predominantly from diverse Boston neighborhoods; 67% are insured through Medicaid, the US health insurance program for low-income individuals and those with disabilities.
Participants were English-speaking adolescents between the ages of 13 and 18 years who owned a smartphone with Internet access, recruited by convenience sampling. Researchers identified potential candidates from the electronic medical record and invited them to participate in the study during a break in their appointment.
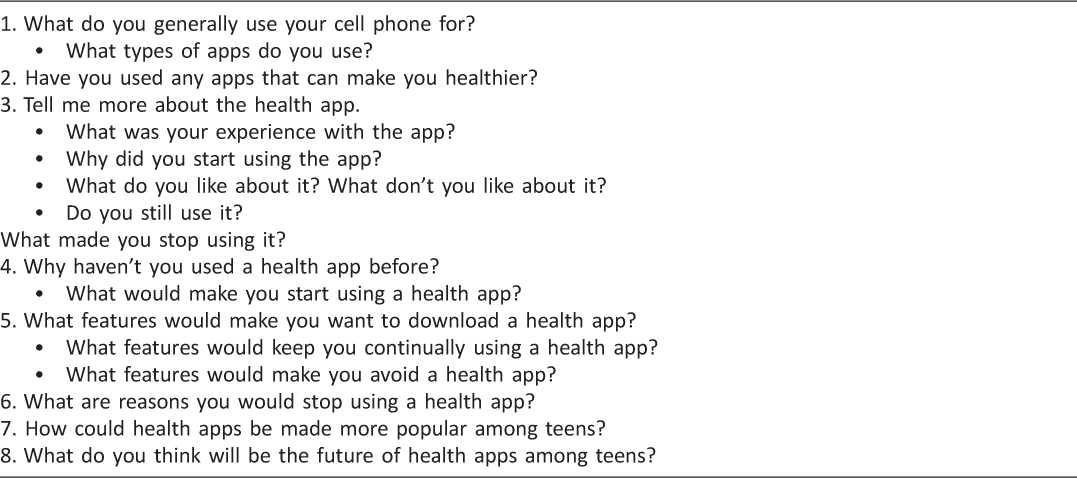
Two researchers obtained written informed consent from parents and assent from adolescents, and then conducted individual semi-structured interviews using a guide developed by the research team (Table 1). The interview guide included a list of questions and topics to be covered during each session; however, conversations were allowed to stray from the guide if appropriate and relevant. The use of the semi-structured guide ensured that collected data was reliable and comparable between sessions.
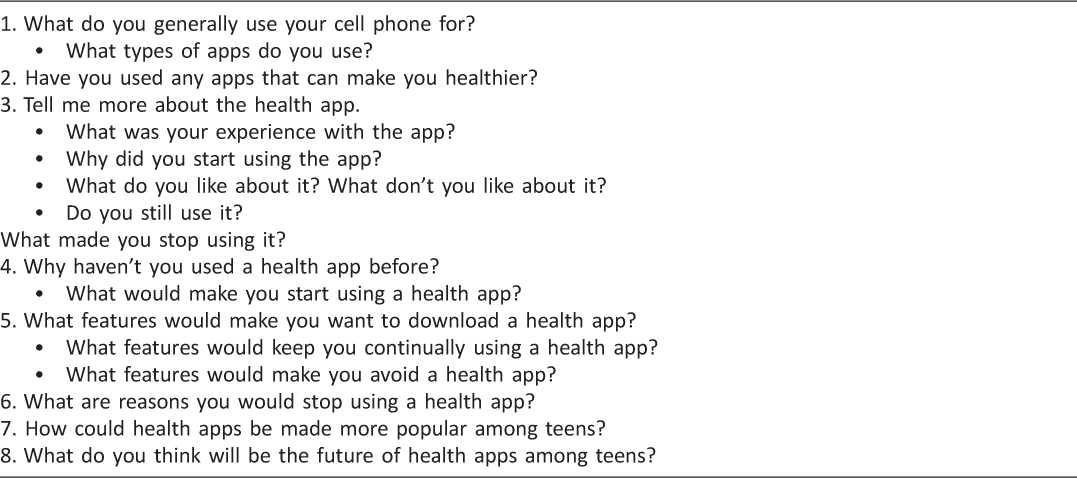
Table 1: Semi-structured interview guide with a list of questions and topics to be covered during each session
Survey question domains included: 1) prior experience using health apps, 2) perceived barriers to, and 3) and facilitators to adopting smart phone apps for health management. To elicit responses to questions in each domain, the research assistants began with general open-ended questions (“What do you generally use your cell phone for?”) then followed with open-ended probing questions (“how, when, where, why”) or specific prompts to encourage participants to provide additional clarifying details when needed. Interviews lasted 10–20 minutes. There was no remuneration for the study, but participants and parents were thanked for their time. Health apps were broadly defined as mobile applications that were aimed towards health promotion, including apps for fitness, diet (nutrition recommendations, calorie counting), behavioral regulation, or carbohydrate counting for diabetes. Adolescents were invited to share their experiences about the various types of apps they had used, thus contributing to a broad inclusion of both health and fitness apps.
The Boston Children’s Hospital Institutional Review Board approved the study procedures.
All interviews were audio recorded and transcribed verbatim. De-identified data was analyzed using inductive thematic analysis. 12 After generating initial codes, in which text segments were attached with labels in order to sort out the data in relation to the research questions; emerging themes or patterns were determined, first independently by two researchers, then collaboratively to establish consistency and validity of findings. As a group, themes were then refined and reviewed to ensure they formed coherent patterns and connected back to the data set. This process was repeated until both researchers were satisfied with the thematic map. Throughout the entire data analysis, any discrepancies were consulted with a third researcher.
Twenty-four candidates were approached, but two were not interested and two did not own a smartphone. The mean age of the 20 study participants was 15.1 years (SD 1.7 years) and 11 were males (55%). Race/ethnicity was divided among 8 Hispanics/Latinos (40%), 10 Blacks/African Americans (50%), 1 White/Caucasian (5%), and 1 Native Hawaiian/Pacific Islander (5%), reflecting the population served by the hospital.
The group of participants as a whole had some familiarity with health-related smartphone apps. Individually, they identified considerable opportunities, barriers, and facilitators related to health app use. These findings were grouped into three major domains—experiences with health apps, barriers to, and facilitators to using health apps—and recurrent concepts were further classified into themes (Table 2).
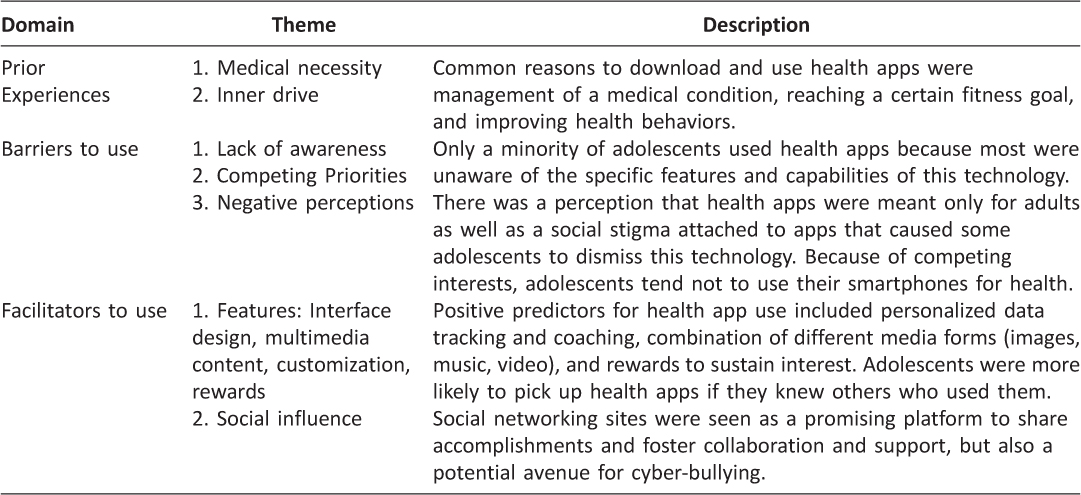
Table 2: Key themes clustered within domains that were identified through inductive thematic analysis of 20 adolescent interviews
Eight participants (40%) had previously used health apps, with six reporting consistent use for at least 1 month. App users reported utilizing them to manage disease, reach a desired fitness goal, or improve health behaviors, such as physical activity or mindful eating. As a matter of fact, one patient with diabetes mellitus and another with attention deficit hyperactivity disorder (ADHD) considered health apps to be essential, medically necessary tools for tracking health conditions. The teen with diabetes mellitus, for example, used an app to calculate the amount of carbohydrates he consumed with each meal, while the participant with ADHD used an app to practice relaxation techniques. Several health conscious users felt that apps aided their inner drive to achieve a certain fitness level. Other individuals found apps to be helpful reminders to stay on track with their health goals. “Everyone has those days when you don’t want to do things. I think baby steps is what it takes, you know, to reach that, you know, just to get used to doing it consistently, and I think that’s when an app can help.”
Out of the eight participants who had tried a health app, two experimented with the app only once before abandoning it. One felt that the app did not enhance her running experience, while the other no longer thought the app relevant to her.
Among the most frequently cited barriers to smartphone health app use was lack of awareness. Three participants had never heard of health apps, and out of the 17 participants who had heard of them, more than half were unaware of their functionalities. Even among owners of phones that came preloaded with a health app, few had opened them. An iPhone owner explained that there were not enough advertisements, promotions, or hype around health apps to stimulate his interest in this type of service. “It [Apple’s Health app] is automatically on my phone, and it was never introduced when I set up my phone… I think if there was more exposure to it, more assistance with it, I think that would encourage users to click on it and actually use it.”
Many adolescents viewed health management as a low priority relative to other interests. One participant attributed this to “all the distractions in the world, on TV, just if we’re just on social media, we get distracted on people’s posts, people’s pictures, people’s comments, celebrities, reality TV.” Many participants reported that they would rather play games, surf the web, or go on social media than monitor their health on a smartphone. Even in the app store, their attention is drawn towards entertainment apps. “I mean, cuz on the app store, all you really look for are music, games, cuz like, I mean, I have a bunch of games there, so that’s really all I look at, unless you’re like in something health, they’re not going to look at anything else.”
Paradoxically, a group of high school athletes interested in physical well-being felt that tracking physical activity on an app was extraneous because they were already exercising. “What I don’t understand is why would you need an app that tell you you’re on a diet if you know that you’re on a diet. Why would you look at the phone every day if you know what you have to do.” These individuals seemed to perceive health apps as a last resort for staying healthy. “If I was to stop playing basketball, then I have no other choice but to work out on the phone.”
Several participants described a social stigma surrounding the use of health apps. One participant thought that using health apps could make teenagers unpopular among their peers. “Some don’t do it cuz they feel other people won’t like it. Some people don’t think it’s cool. That’s why they don’t use it. They’re afraid if they use it, someone might make fun of them.” Strategies suggested by participants to combat these negative perceptions included using celebrity endorsements and marketing through social media.
A commonly held belief was that health apps were meant only for adults. “Well, like more so adults that like to work out a lot–they may use this app to help them.” Negative comments about health apps included “it wasn’t physically appealing” and “this thing, like is boring and dull for a teenager’s use [and] is really complex. One participant was dissuaded by how difficult it was to navigate the app. “I looked at it and one, I didn’t know how to use it so I just didn’t bother with it.”
Several participants were enticed by an app because of its “look and feel.” “Well it looks really, I dunno, it looks really cool. It looks pretty modern, sleek, so that’s why I like using it.” Apps that were simple to use and visually appealing with vibrant colors, bold graphics, animation, and videos piqued some health app users’ initial interest. Various participants recommended adding music features and game components to the app, such as giving prizes or points for achieving certain tasks, creating exercise competitions between friends, and incorporating virtual adventures that require exercise.
Apps that enabled customization, such as goal setting, personal data tracking, and tailored messaging, were universally deemed important by participants. An adolescent who used an app with a step counting feature said it motivated him to work harder each day. “I actually want to exercise more. Like before, I’ll stick around and play video games. Now, I want to get my steps more than yesterday or the day before. I want to progress more.” Others mentioned that real-time feedback on biometric data, like heart rate and calories expended, encouraged them to increase physical activity in their day. “I like that it like could tell you what is going on with your heart… It’s a cool app because it encourages me to do exercise more.”
Some participants wanted calorie counting so they would know how many calories they were consuming and burning so that they could adjust their portion sizes, diets, and physical activity levels. However, not everyone felt that calorie counting was a desirable feature because weight was a sensitive issue that adolescents might not be ready to tackle on a smartphone app. “I think like telling you your weight, that’s something. Don’t do that. Don’t do that. I think that’s the biggest one, the weight thing.” Such strong emphasis on weight could lead to stigma and weight shaming from fellow adolescents, as noted by a participant, “I don’t think they should post online how many calories they burned or something since some of that can get bad cuz then it could start cyber-bullying online.”
Several participants felt that a “virtual health coach” app would push them towards achieving their personal health goals. For example, participants wanted apps to give them diet and exercise recommendations. “Um, like just letting me know how much I can do. Just lose weight, how fast I can get it done. How much time it would take to get to the goal. Uh like certain number of calories per week.”
Intrinsic motivation appeared to be an important factor among teen app users. One adopter said he used health apps to achieve a desired, pre-set goal. “Cuz I would wanna know everything I can do possible, so give me all that you can tell me how to help me reach my goal, cuz that’s where I wanna get.” For several others, this intrinsic motivation appeared rooted in a desire to keep a medical condition under control. The participant who had ADHD, for example, used an app to guide him through breathing and relaxation techniques whenever he felt agitated. If he did not use the app, he “got kinda cranky.”
To help engage those with lower intrinsic motivation, participants suggested incorporating tangible rewards such as gift certificates, food baskets, or workout equipment, to externally motivate the completion of targeted health behaviors. Others suggested rewards in the form of app store credit or virtual points that could lead to actual, physical prizes to reinforce the completion of positive health behaviors.
Participants reported that seeing or hearing other individuals use health apps would influence their own decision to adopt them. Celebrity endorsements could garner interest among teens, which one participated noted, “I know kids are influenced if a lot of people using it are like famous or popular.” For example, “if Kobe Bryant or Lebron James were using it, I think that would encourage more teenagers to use it.” Physicians could also play an influential role. Some participants reported they would start using a health app if their doctor recommended it. Certainly, peer pressure could affect teens’ decisions to pick up new habits, like using health apps. One participant explained how he convinced his baseball teammates to start using a health app, and this subsequently led to a fun competition between them during practice. “I actually got four friends download it the other day. Yeah, cuz it tells you how many steps, we were on a run in baseball, so like, look, I took more steps than you.”
Social media sites, like Facebook and Twitter, were also viewed as practical platforms to bring awareness to apps. “You have to get something that’s going to catch a kid’s eye and then it will be word of mouth. One kid loves it, they tell their friends about it. Then that’s when it becomes on social media.” Social media can also showcase individual achievements, which in turn might generate healthy competition and collaboration among peers. Two participants found that posting their fitness accomplishments on social media instilled a sense of personal accomplishment and motivation to keep exercising. Additionally, social media could be used to share health information with others as well as promote unique features of the apps. “I think that if, let’s say you achieve a task, achieve walking a mile, if you can share that with your page or your friends online, that can encourage others to use the app. It could encourage them to want to do something more active and eat healthier=.” However, despite its various suggested benefits, some participants feared that linking social media to health apps could contribute to cyber-bullying or promote excessive exercise.
In this qualitative study, we examine prevailing beliefs regarding the use of smartphone applications for managing health among adolescent patients seen for routine care at a large urban pediatrics clinic in Boston. Our findings suggest that, despite the rapid proliferation of mobile health technology, uptake of smartphone health apps remains low among youth. Nearly two-thirds of teens in our study had never used a health app, and one-fourth of them had not even heard of health apps. Our results are consistent with recent statistics showing that only 21% of teenage smartphone users aged 13 to 18 years downloaded mobile health apps and of those, only 8% used them regularly. 13
In our study, we found that lack of awareness, even among owners of sophisticated smartphones, was an important deterrent to using health apps. Additional adoption barriers included the widely held perceptions that health apps were “boring,” “meant for adults,” or “a last resort to staying healthy.” Participants were particularly concerned about the opinions of their peers and worried that they would be branded as “losers” for using health apps. Competing priorities were a further obstacle to sustained health app use. Youth said they had better uses for their time and preferred using their phone to text friends, play games, or watch videos. However, adolescents diagnosed with chronic medical problems presented a notable counterpoint and perceived health apps as indispensable tools to help them manage their conditions.
We also learned that engaging app features, such as user-friendly interfaces and multimedia content, were important facilitators of health app adoption among teens, while personalized tracking and tangible rewards sustained usage to reinforce desired behaviors. Social influence was another major facilitator of health app adoption and use among adolescents. Adolescents reported being more likely to try a particular health app if a friend, doctor, celebrity, or networks on social media recommended it to them.
In consideration of these findings, we synthesized potential strategies to promote the use of health apps among adolescents: 1) incorporate features that appeal to adolescents and 2) use social media to build awareness and a community of users.
In a digital age when teenagers are spending substantial amounts of time using media—texting, social-networking, watching videos, and gaming—health apps need to be fun and entertaining for teenagers to use them.
“Gamification” or the integration of game elements into apps was embraced by many of our respondents as a strategy to counteract the negative perceptions surrounding health apps. With nearly three-quarters of teens playing games online or on their phones, 2 the integration of game elements, such as virtual badges, leaderboards, points, and challenges, into health apps could draw interest from a wide adolescent audience. 14 Furthermore, research already suggests that electronic games can improve physical activity, health education, and disease self-management outcomes. 15
Beyond entertainment, games may also promote intrinsic motivation. According to self-determination theory, people are naturally driven to pursue new experiences for personal growth and fulfillment. 16 Since gamification can integrate new challenges or health tasks into apps, users’ innate desire to conquer them could be harnessed. Tangible, extrinsic rewards in the form of gift cards and app store credit, as suggested by our participants, could also be linked to games, which studies have shown, may help attain health outcomes that would not ordinarily be achieved with intrinsic motivation alone. 17
As our study further suggests, the “look and feel” of an app can pique teens’ initial interest. Colorful images, animation, and popular culture references may increase appeal to teens. Multimedia content with videos (e.g. instructional videos for exercise or cooking) and music (e.g. music that syncs to workouts, platform for free music) could keep apps entertaining.
Personalized features, such as having a “virtual trainer” that provides individualized exercises, diets, and advice could inspire healthier habits as it caters to users’ specific goals and lifestyle. While counting calories may be desirable by some users, a strict focus on body weight could have detrimental consequences. Studies show that the stigma, excessive exercise, and teasing resulting from weight preoccupation can contribute to depressive symptoms. 18 , 19 Additionally, a strong emphasis on weight may propel teenagers who are weight- or image-conscious to attempt extraneous exercise or dieting with potential serious risks. 20 Therefore, we recommend that health apps steer away from a narrow weight-focus and instead target lifestyle behaviors conducive to optimal health.
In summary, health apps should be entertaining, visually appealing, user-friendly, and customizable to suit personal interests and preferences. Because teenagers are at a pivotal time of development as they begin making their own health decisions, apps that enable goal setting and health tracking could provide teens with more autonomy over their health.
Given that lack of awareness appears to be a primary reason why few teens use health apps, social media could bring widespread awareness and interest to this novel technology. According to a recent poll, 41% of consumers said social media would affect their choice of a specific doctor, hospital, or medical facility. 21 With 76% of teens on social media, 2 platforms like Facebook and Twitter have potential to reach a broad adolescent audience while addressing misperceptions about health apps.
Social media also provides a vehicle to integrate marketing strategies, such as audience segmentation, to target populations that are traditionally not reached by the medical system. 22 Since teens prefer visuals, music, comedy, and popular culture; marketing health apps with these interests in mind could potentially entice naïve users and reshape any preconceived attitudes about apps. 23
Connecting social media with health apps can also foster a sense of community among users. A prior study illustrated how creation of a mobile virtual community in overweight individuals allowed them to gain increased social support because they could seek out one another for advice and encouragement. 24 Social media can also provide easier platforms to share information and words of encouragement, 25 which our interviews noted. Further evidence shows that peer driven information exchange can create empowered patients who learn how to manage their health from others sharing the same conditions. 26 The fitness tracker, Fitbit, is a prime example of how social media conversations can breed success. According to a report by Kantar Media, one of the primary reasons for Fitbit’s unmatched success in the wearable fitness device market is its high volume of users who share their achievements on Twitter. 27
A major strength of this study was its qualitative research approach. Conducting individual interviews allowed participants to openly share and elaborate their thoughts. As a result, we were able to capture insightful and nuanced perspectives from a diverse adolescent population representative of the demographic served by many safety-net health care institutions. Although a reasonable number of interviews were conducted, two-thirds of participants had not had meaningful experiences with a health app; as a result, these discussions were limited to hypothetical situations, so their input may not accurately portray how apps are actually used. In the future, trigger materials or prototypical apps can be provided to prompt further discussion. Future studies can also capture a broader adolescent population to gain unique perspectives towards health apps in relation to weight and health status.
Over the past several years, there has been an explosion in mobile apps for health, yet the majority of apps are not tailored to the younger, tech-focused generation. The insights gathered in this study can aid diverse stakeholders involved in adolescent health. Developers can incorporate app features proposed in this study to design apps that are practical and desired by their target audience. App designers can also assist in the overall design of health apps to make them “hook” people in the same way that entertainment does. Pediatricians and other healthcare professionals can use their influence to promote tried and tested apps to patients, while also helping them understand how this technology may pertain to their lives. Adolescents have a responsibility to start learning how to take care of themselves—health apps give them the opportunity to put health into their own hands. As research for mobile health apps continues to grow, we believe that they will one day be part of standard care.
AC and RK equally contributed to the conception and design of the study, acquisition of data, analysis and drafting of the manuscript. JC is the Principal Investigator and assisted in the interpretation of the data and provided substantial guidance and input during the revision of the manuscript. All authors approved the final version of the manuscript.
The authors have no competing interests. All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
This research was partly supported by internal funding from the Division of General Pediatrics, Boston Children’s Hospital.
The Boston Children’s Hospital Institutional Review Board approved the study procedures.
The authors would like to thank the patients and families at Boston Children’s Hospital Primary Care Center at Longwood for donating their time towards this project.
1. Pew Research Center. The Future of Apps and Web. Available at: http://www.pewinternet.org/2012/03/23/the-future-of-apps-and-web/. Accessed on September 6, 2015.
2. Pew Research Center. Teens, Social Media & Technology Overview 2015. Available at: http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/. Accessed on September 6, 2015.
3. Pew Research Center. Teens and Mobile Apps Privacy. Available at: http://www.pewinternet.org/2013/08/22/teens-and-mobile-apps-privacy/. Accessed on September 6, 2015.
4. World Health Organization. mHealth: New horizons for health through mobile technologies. Available at: http://www.who.int/goe/publications/goe_mhealth_web.pdf. Accessed on September 6, 2015.

5. Tang J, Abraham C, Stamp E, et al. How can weight-loss app designers’ best engage and support users? A qualitative investigation. British Journal of Health Psychology 2015;20(1):151–71.

6. O’Dea JA. Why do kids eat healthful food? Perceived benefits of and barriers to healthful eating and physical activity among children and adolescents. J Am Diet Assoc 2003;103(4):497–501.
7. Krebs NF, Himes JH, Jacobson D, et al. Assessment of Child and Adolescent Overweight and Obesity. Pediatrics 2007;120(Supp 4):S193–S228.

8. Payne HE, Lister C, West JH, et al. Behavioral Functionality of Mobile Apps in Health Interventions: A Systematic Review of the Literature. JMIR mHealth uHealth 2015;3(1):e20.
9. Wieland LS, Falzon L, Scimamanna CN, et al. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochraine Database Syst Rev 2012;8:1–143.

10. Hermawati S, Lawson G. Managing obesity through mobile phone applications: a state of the art review from a user-centred design perspective. Pers Ubiquit Comput 2014;18(8):2003–23.

11. Lubans DR, Smith JJ, Skinner G, et al. Development and implementation of a smartphone application to promote physical activity and reduce screen-time in adolescent boys. Frontiers in Public Health 2014;2:42.

12. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3(2):77–101.
13. Wartella E, Rideout V, Zupancic H, et al. Teens, Health, and Technology: A National Survey. Evanston, IL: Center on Media and Human Development, School of Communication, Northwestern University; 2015.
14. Miller AS, Cafazzo JA, Seto E. A game plan: Gamification design principles in mHealth applications for chronic disease management. Health Informatics J 2014;1–10.

15. Primack BA, Caroll MV, McNamara M, et al. Role of video games in improving health-related outcomes: a systematic review. American Journal of Preventive Medicine 2012;42(6):630–8.

16. Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum Publishing Co; 1985.

17. Deci EL. Effects of externally mediated rewards on intrinsic motivation. Journal of Personality and Social Psychology 1971:18;105–15.

18. Landoll RR, La Greca AM, Lai BS, et al. Cyber victimization by peers: Prospective associations with adolescent social anxiety and depressive symptoms. J Adolesc 2015 Jul;42:77–86.

19. Carpenter LM, Hubbard GB. Cyberbullying: implications for the psychiatric nurse practitioner. J Child Adolesc Psychiatr Nurs 2014;27(3):142–8

20. Stein K. Severely Restricted Diets in the Absence of Medical Necessity: The Unintended Consequences. J Acad Nutri Diet 2014;114(7):986–94.
21. Ottenhoff M. Infographic: Rising Use of Social and Mobile in Healthcare. The Spark Report; 2012. Available at: http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed on September 6, 2015.

22. Evans WD. How social marketing works in health care. BMJ 2006;332(7551):1207–10.
23. Akcay O. Marketing to Teenagers: The influence of Color, Ethnicity and Gender. International Journal of Business and Social Sciences 2012;3(22):10–8.

24. Fukuoka Y, Kamitani E, Bonnet K, et al. Real-time social support through a mobile virtual community to improve healthy behavior in overweight and sedentary adults: a focus group analysis. J Med Internet Res 2011;13(3):e49.

25. Vandewater EA, Denis LM. Media, social networking, and pediatric obesity. Pediatr Clin North Am 2011;58(6):1509–19.

26. Wong CA, Merchant RM, Moreno MA. Using social media to engage adolescents and young adults with their health. Healthcare 2014;2(4):220–4.

28. Dute DJ, Bemelmans WJ, Breda J. Using Mobile Apps to Promote a Healthy Lifestyle Among Adolescents and Students: A Review of the Theoretical Basis and Lessons Learned. JMIR Mhealth Uhealth. 2016 May 5;4(2):e39.

29. Direito A, Jiang Y, Whittaker R, Maddison R. Apps for IMproving FITness and Increasing Physical Activity Among Young People: The AIMFIT Pragmatic Randomized Controlled Trial. J Med Internet Res. 2015 Aug 27;17(8):e210.